Theresa Brown, RN, is an oncology nurse and one of the very few nationally prominent nurse-writers in the areas of nursing and health care. She on the Center’s Advisory Council and this is her first post as a HealthCetera guest blogger.
 Being the “nurse who writes” means I work under a misconception. Although a number of physicians regularly opine on the work they do in books, articles in The New Yorker, and my own home base The New York Times, I’ve never heard the MD-writer combination described as odd or bewildering. However, being an RN-writer is seen as unusual, and my admittedly unusual academic background—I have a PhD in English from the University of Chicago —- contributes to the view that I’m an intellectual oddity among my nursing peers.
Being the “nurse who writes” means I work under a misconception. Although a number of physicians regularly opine on the work they do in books, articles in The New Yorker, and my own home base The New York Times, I’ve never heard the MD-writer combination described as odd or bewildering. However, being an RN-writer is seen as unusual, and my admittedly unusual academic background—I have a PhD in English from the University of Chicago —- contributes to the view that I’m an intellectual oddity among my nursing peers.
But I am not alone in combining nursing and writing. Many nurses will be familiar with Echo Heron’s nursing memoirs and Carol Gino’s The Nurse’s Story. Tilda Shalof, a Canadian ICU nurse, and Patsy Harman, a certified nurse midwife, are both nursing and writing right now, and Harmon’s new novel, The Midwife of Hope River was just released. Saving Lives: Why the Media’s Portrayal of Nursing Puts Us All at Risk, a polemic by Sandy Sommers, RN, MSN, MPH powerfully argues that media stereotypes of nurses dangerously undermine nursing’s professional legitimacy.
These nurses, and I, all write for the same reasons that physicians do: educating the public about how health care works, outlining ways to make health care better, exploring how hard it is to work in a job that often deals with death, or showing what nurses’ clinical work actually involves.
By writing about nursing (or medicine) we learn about the nature of our roles as caregivers and we communicate the importance of that role to readers. In a recent column entitled “Money or Your Life” I wrote for The New York Times, I argued in favor of the Affordable Care Act by telling the story of a patient who wished for a death panel because he had no health insurance and worried that the care he needed to save his life would bankrupt his family. His choice would have been for the government to kill him rather than for his family to become destitute financing his care.
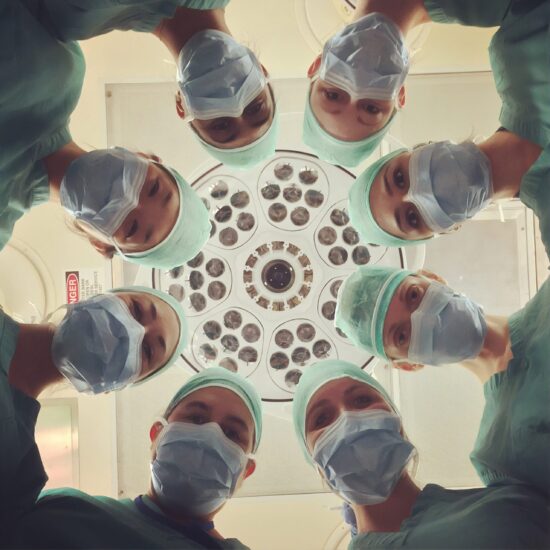
He asked me, his nurse, about death panels. That was, perhaps, not something he would have asked his physician about, or at least in this case it wasn’t an issue he had raised with his doctor. Nurses spend the most time with patients of any hospital staff and we often serve as intermediaries between the patient and everyone else, and this column highlighted the importance of the nurse’s intermediary role. The patient told me about his financial worries. I told the rest of his medical team, the social worker, and his care coordinator, and then everyone put their heads together to figure out how to best help this particular patient.
It’s a horrible story with a potentially positive resolution. If I, the nurse, hadn’t been there to listen, and then emphatically communicate what I heard from this desperate patient, the story might in the end have been thoroughly horrible. Perhaps the patient would have refused care, or his family might have suffered in silence. And although his financial concerns might have been addressed at another time, in that moment I heard and acted. That’s part of what nurses do, and it’s important to have nurses’ voices out in the world explaining that this is just one reason why we are valuable to patients.
Here at Hunter College, the Center for Health Media and Policy is attempting to prepare more nurses to get our stories out into the world via their “Narrative Writing Program.” Run by Senior Fellows Joy Jacobson and Jim Stubenrauch, the CHMP Narrative Writing Program gives nurses tools for writing about work and, perhaps even more importantly, helps them feel comfortable with the idea of themselves as nurse-writers who can contribute to conversations about health care policy. The courses taught by Joy and Jim are not about journaling in a vacuum. The point of nurses learning how to write essays, blog posts, poems, columns, and policy analyses is to reveal the emotional and physical realities of nursing to readers who are unaware of those realities and whose lives will, at some time, be affected by them.
For example, referring back to my own writing, I’ve authored columns on the need for safe staffing ratios and the problem of physician bullying. In both instances my motivation was concern for patients’ safety and I had anecdotes that made clear how these issues affect quality of care. I brought in data for both columns, too, but while data is important, it’s the anecdotal evidence gleaned from my perspective as a bedside nurse that really made the columns persuasive.
I wasn’t a writer before I became a nurse. I was an academic, and I had taught composition, but only after I became a nurse and then began, almost by chance, writing about nursing, did I find the writerly voice I now have.
Whenever people tell me that combining writing and nursing is . . . unexpected, I want to tell them about all the great nurse-writers out in the world. Whether you’re posting on a blog read by three people, or writing your third book, we nurses have a lot to say. It’s time for more of us to start writing down our thoughts and experiences, and then share them with an interested public.






Katie / September 28, 2012
I agree completely! Also, I found that writing was actually therapeutic for me during nursing school, I don’t think I would have survived without my blog!
/
Thomas Lawrence Long / September 28, 2012
Nurse writers might benefit from visiting NursingWriting.com, a Web site that encourages nurse writers and writing. Despite its dot-com domain, NursingWriting is not for profit, supported by the School of Nursing at the University of Connecticut.
/
Thomas Lawrence Long / September 28, 2012
There is now a Wikipedia entry for “Nurse writer” (as a companion to one that was first published several years ago for “physician writer”). It is not complete, so readers are welcome to add new authors and develop existing ones.
http://en.wikipedia.org/wiki/Nurse_writer
/
Patricia Wagner Dodson / September 28, 2012
I believe that when nurses write, they are not only telling their own stories but the stories of their patients, and those stories need to be told. I work at a cancer center, and over the last few weeks the main entrance to our cancer center has been closed for construction, and the patients have been walking through a long corridor that leads straight through the offices of about a dozen research nurses. I have found this experience fascinating. I thought I knew what my patients went through, but I tend to see them individually, not collectively. Most of the nurses have made a point of keeping their doors closed. I have kept mine open. I want to see the hundreds of people who walk by my door–the patients and their loved ones who push them in wheelchairs or walk slowly next to them. It breaks my heart to see how much they are loved, and how much they struggle to get to their treatments, to keep going forward with their lives. I believe that what I have seen needs to be shared and that by sharing these stories, we have the opportunity to shape changes to the way our country has practiced medicine.
/
suki / September 30, 2012
Whoever said it was totally correct: Nurses have a lot to say. How many times I am ready to explode, wanting someone to know what we actually experience in a day at work? I cannot begin to verbalize my own words at times. In talking with some coworkers, I often find they are themselves struggling with feelings and emotions due to our workplaces. However, us nurses often lock our feelings and thoughts of injustice aside. Why? Because of fear. Now, I’m not talking those past memories that bring a smile to our faces. I’m talking the real deep issues and horrible things we witness and must somehow come to terms with while at work. So many nurses have developed a mechanism for shutting off their feelings, their caring and push those things out of their mind. Why do we do that? We have a lot to say yet we don’t say anything.
/
josephineensign / September 30, 2012
Thanks for this post Theresa–and thanks to the other people who have left thoughtful comments. What’s left out of the discussion (except off the record/behind closed doors) is that nurses who write about their work/their patients are often threatened with disciplinary action by their employers. I’m beginning to suspect that’s why there are so many nurse poets and nurse fiction writers. They can more easily disguise their real work, real stories, and keep their day (or night) jobs. Even in my academic job I have been ‘nudged’ at times to cease writing (as in ‘real writing’). I recognize that I have a relatively privileged position (tenured) and can ignore the ‘nudges.’ Many other nurses in hospital, clinic, community and other settings do not get to play the tenure card.
And thank you Dr. Long for adding “nurse writer” to Wikipedia. I wrote a blog post on that today and included a list of my recommendations for nurses who want to write: “Nurse Writers Arrive in Wiki-land” at josephineensign.com.
/
Thomas Lawrence Long / October 2, 2012
One of the more common ways of communicating with the public or with opinion shapers is the newspaper letter to the editor or op-ed essay. Nurses need to move from silence to voice (as Buresh and Gordon frame it). Not sure how to write a letter to the editor or op-ed essay? Go here: http://nursingwriting.wordpress.com/2012/08/23/writing-letters-to-the-editor-editorials-and-op-ed-essays-part-i/
/
TheNerdyNurse / October 5, 2012
You did not mention the fear that many nurses have for retaliation from their employers. There are many nurse bloggers who write anonymously because off their employers misunderstanding of social media. Dare I say that if healthcare organizations would stop making nurses who write feel threatened then you might see a whole new drop of nurse writers start to blossom.
Great article.
And for the record, I’m terrible at spelling and grammar, so it has been difficult for me to get over the fear of being mocked for making an error in a public domain.
/
lilk8tob / October 5, 2012
Great point!
/
Jennifer Olin, RN / October 5, 2012
Writing about nursing, the education, the profession, the responsibilities, and where it all fits into daily life has been an evolutionary experience for me. For the past year I have had the privilege of writing about nursing and in that year I have grown as a nurse. I have recalled subjects from nursing school I never thought I would think about again. I have seen where we as nurses fit into history, art, science, politics, and business. I have learned and relearned the power we have and the power we could generate if we pulled together and I have written about the damage we can do when we pull each other apart. As nurses we have a voice and we need to share it with our colleagues, nurses of the future, and every person out there who has had or will need our skills and our services. My fellow nurses always seem amazed that I write; I wish they all would.
/
bethboynton / October 9, 2012
Thanks Theresa for this excellent article and our colleagues for such great discussion. In my experience, as a nurse consultant, speaker, and writer it can feel risky to be totally honest! Like Britney Wilson says, we may worry about job loss. Sad but true. More and more I am finding my own voice. I believe empowering ourselves, each other and consumers is something nurse writers are doing from all sorts of different perspectives of healthcare. This work is so vital to healthcare reform. Ultimately, it is an honor to be a nurse writer!
/