
 Ann Campbell, RN-BC, MPH is a hospice nurse at an inpatient palliative and hospice care program in New York, and is currently an NP student at Hunter Bellevue School of Nursing. She is a research associate for the CHMP.
Ann Campbell, RN-BC, MPH is a hospice nurse at an inpatient palliative and hospice care program in New York, and is currently an NP student at Hunter Bellevue School of Nursing. She is a research associate for the CHMP.
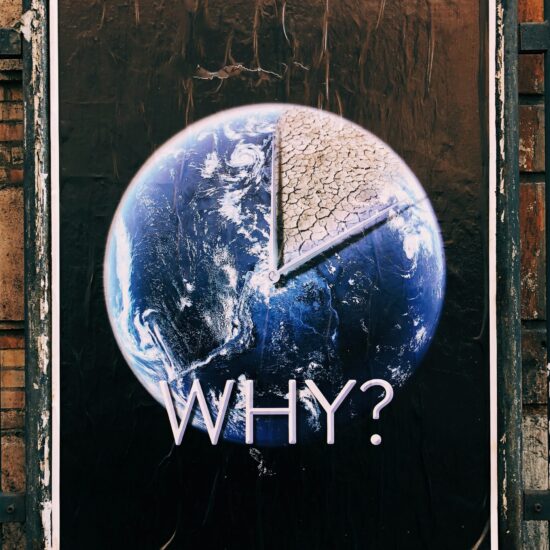
You’re going to die.
It’s the statement none of us want to hear, but at some point will all face, even if it’s directed to a loved one: “we’re going to lose him” or “he’s gone.”
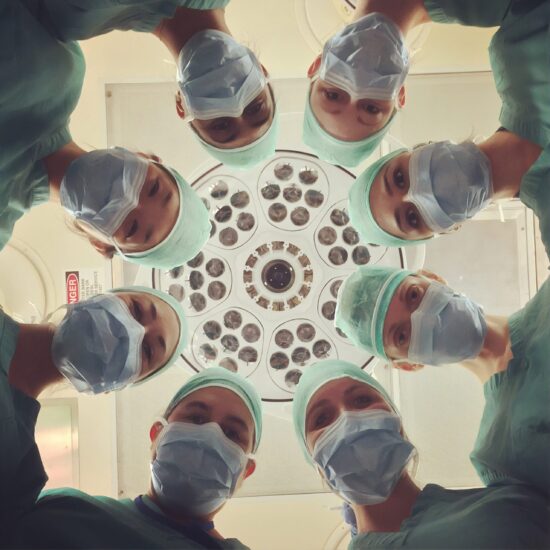
As a hospice nurse and nurse practitioner student I see that all too often, this discussion occurs when death is imminent, even though the writing has been on the wall for some time. Naturally, patients and families hold out for a cure as the odds of survival fall precipitously. Every failed intervention may bring new side effects, suffering, and a stronger medicine. As alternatives dissipate, the hope for a miracle cure grows. Finally, after numerous hospitalizations, difficult interventions, and toxic drug regimens, if patients are lucky a physician will prepare them and their families for a death that may come in days, possibly hours. The loved one continues to receive medications for symptom mitigation in the days that follow. Families and patients alike are distraught, confused, and frustrated. There is not enough time to adjust to this new reality. Although patients are often comfortable at the end thanks to the hospice nurses and medications, could we have done better?
Palliative and hospice care is often left for the very end of life. However, a new study of Nurse Practitioners integrating palliative care into a primary care model confirms the benefits of early integration. This is shown to reduce emergency department visits and improve symptoms, which increases time at home and quality of life.
Our health care system faces the challenge of allocating limited resources to an aging population. The focus is on solutions that improve patient quality of life while minimizing unnecessary expenses. One proven way to achieve these dual goals is for Nurse Practitioners to actively integrate palliative care into the health care system at an earlier time.
I’ll never forget one patient I cared for. When diagnosed with a terminal form of cancer he went on vacation. He and his wife circumscribed the earth because they knew their time was limited, and they wanted to make it count. In the clinical realm, the same type of patient is often treated despite inevitable failure, and harsh side effects from medications. Perhaps earlier discussions about death will help more people maximize the time they have with their loved ones, and decrease unnecessary waste in a system with finite resources.






Rosalie Galante / October 1, 2012
Well said Ann. As Hospice nurses we have the inside knowledge of how to help patients have “a good death”. The challenge is how to get the word out to the masses.
/
rehabilitateyourheart / October 3, 2012
I too have watched many patients kept alive through medical procedures and pharmaceuticals only to have a miserable quality of life and go broke doing so. I too strongly believe we need to utilize our palliate and hospice care much earlier. Keep up the good work!
/
Diane Hughes / October 4, 2012
I agree, Ann. It would better serve the patient and family if we prepare them earlier for the inevitable. We are very much still a death defying society. The issue lies deeper than palliative care as I feel how one is prepared for the dying process lies in the roots of ones culture. How we view death as a continuum of our life span is worth looking at across different cultural lines. It’s what we learn from that which will gradually change our perception of the inevitable.
/
annharpercampbell / October 4, 2012
Yes, how to get the word out in a death defying society. This is one of the reasons I appreciated the study of Nurse Practitioners integrating palliative care into primary care. Maybe the approach will get the word out, and have an impact on society.
I have also been struck by the negative connotation of “hospice”, and “palliative care” held by members throughout the health professions. Many see hospice as a place to die; however, in my experience I have seen it as a place to live. There exists a different kind of support; one that breeds a more eternal hope. An article that recently came across my desk has encouraged this view, and I will share it with you soon.
/
Billy Rosa / October 7, 2012
Brava, Ann! I love this and you are right – it is about living, it is not about dying. It is ALWAYS about living. HOW and with what quality and with what powers of choice I wish to live! People don’t understand that because they allow their fear rather than their love to overtake and navigate their perception of their remaining time. Dovetail this with the pervasive belief that death need not exist and you have yourself full-fledged denial. Not only is it our responsibility to chip away at these cultural norms but to do so in a way that promotes authentic human caring and creates healing environments for us and our patients
/
Lee Brando / August 20, 2016
This is a great article.
I am a graduate student at The New School for Social Research and my area of interest is End-of-Life care. Particularly, I am concerned with nurses’ perspectives on medically assisted death in states, like New York, where physician assisted death has become an important political issue. I’m interested in talking to nurses because their perspective is not heard as frequently when compared with that of physicians; and, they offer a unique perspective, spending more time with patients and getting a fuller picture of patients as well as families at critical times.
If you are interested I would like to speak with you about your thoughts and experiences on this matter. I can accommodate your schedule by speaking to you by phone and the interview can be as long or short as you wish. If you are not able to speak with me, I would greatly appreciate if you could let me know of someone who might be.
Much appreciation for your consideration,
Lee Brando
MA, Medical Anthropology, University of Colorado at Denver
/