This guest post is written by Ashly E Jordan, a DPH Candidate at the City University of New York.
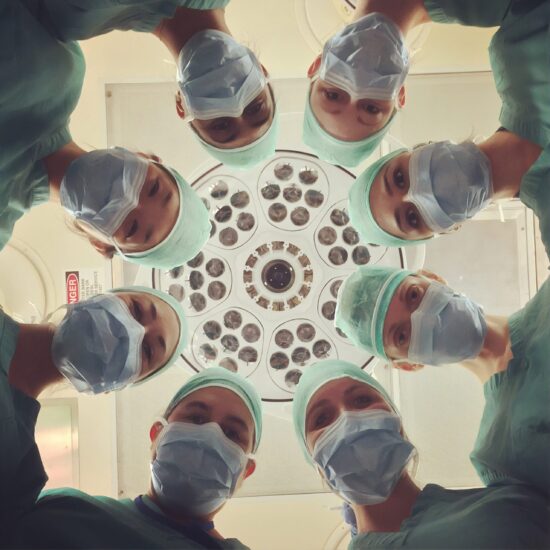
 It was a relatively small abscess at the base of Angel’s wrist. Angel lived in an abandoned building in Southwest Detroit. Angel was a long-term drug user. Angel was a citizen, but had little schooling and was predominately non-English speaking. She was born in and grew up in Chicago. Angel came to the syringe exchange program where I was working, and presented with the abscess. We referred her to the nearest clinic, which in this impoverished neighborhood was almost an hour’s walk. Such abscesses are common in drug injectors and can generally be treated easily and inexpensively as an outpatient. Angel did not have a car, and did not have bus fare. She did walk to the clinic, only to be turned away. While Angel had Illinois Medicaid, the clinic would not see her because they saw patients only with Michigan Medicaid. She had previous bad experiences with perceived discrimination and stigmatization in other care settings, and being turned away felt normal. She did not know she had other options. Angel was soon admitted to the hospital and was found to have an infection that had spread to her blood (she had “sepsis”). She required a month long hospitalization, and two surgeries on her arm before she was eventually released alive but with enormous permanent scars on her arm. Angel had health insurance and would be considered by many to have “health care access,” however due to multi-level barriers including stigmatization, lack of transportation, arcane insurance restrictions and regulations, to her own learned fatalism, Angel’s inexpensively and easily treatable abscess came to require a month-long hospital stay with both worse clinical outcomes and vastly greater societal expense.
It was a relatively small abscess at the base of Angel’s wrist. Angel lived in an abandoned building in Southwest Detroit. Angel was a long-term drug user. Angel was a citizen, but had little schooling and was predominately non-English speaking. She was born in and grew up in Chicago. Angel came to the syringe exchange program where I was working, and presented with the abscess. We referred her to the nearest clinic, which in this impoverished neighborhood was almost an hour’s walk. Such abscesses are common in drug injectors and can generally be treated easily and inexpensively as an outpatient. Angel did not have a car, and did not have bus fare. She did walk to the clinic, only to be turned away. While Angel had Illinois Medicaid, the clinic would not see her because they saw patients only with Michigan Medicaid. She had previous bad experiences with perceived discrimination and stigmatization in other care settings, and being turned away felt normal. She did not know she had other options. Angel was soon admitted to the hospital and was found to have an infection that had spread to her blood (she had “sepsis”). She required a month long hospitalization, and two surgeries on her arm before she was eventually released alive but with enormous permanent scars on her arm. Angel had health insurance and would be considered by many to have “health care access,” however due to multi-level barriers including stigmatization, lack of transportation, arcane insurance restrictions and regulations, to her own learned fatalism, Angel’s inexpensively and easily treatable abscess came to require a month-long hospital stay with both worse clinical outcomes and vastly greater societal expense.
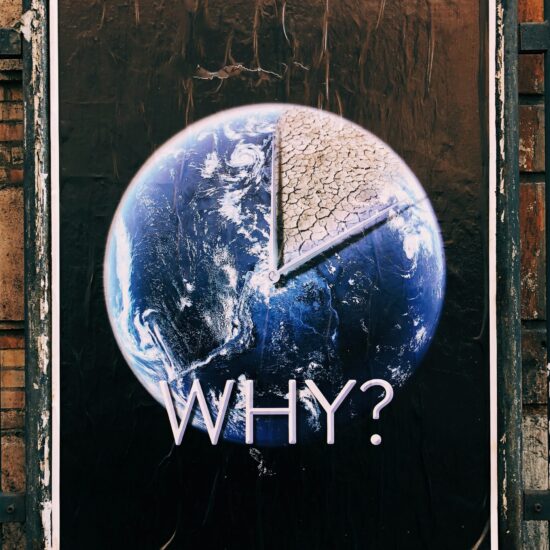
The Affordable Care Act (ACA) seeks to improve health care in the U.S. by broadening the base of those who are insured. We spend more per capita on healthcare than any other country in the world yet millions of citizens lack health insurance and key indicators of national health, such as infant mortality and life expectancy, are lag many other nations. The ACA will expand coverage by requiring insurers to, for example, cover children of insured parents through 26 years, to accept those with pre-existing conditions, and by expanding Medicaid to all individuals under 65 below 133% of the federal poverty level. It is commonly assumed that ensuring individuals gain “access” to health care, with “access” defined as being insured, will alleviate disparities in care. Yet having insurance is only one of many factors required for people to receive needed care. Insurance coverage is necessary, but by itself is not sufficient.
Financial considerations and the affordability of insurance represent major barriers to care that are partially alleviated by the implementation of health insurance coverage through the ACA, but many barriers to actual “access to care” remain unresolved under the ACA. Such barriers to care include: geographic access (e.g., transportation), availability of sufficient numbers of qualified providers (e.g., wait time; complexity of treatment management) and acceptability of care settings (e.g., stigmatization; cultural attitudes / norms). All have been empirically demonstrated to contribute to delayed diagnosis and initiation of treatment for conditions such as post-traumatic stress disorder; hepatitis C (HCV); and depression.
In response to these disparities, interventions targeting these additional critical aspects influencing receipt of care have shown considerable success in improving health outcomes among those insured. For example, hiring culturally sensitive providers to treat patients in clinical settings and offering patient navigation services for particularly complicated disease states including cancer, HIV and HCV have improved utilization and continuation of care.
The ACA is an important step in expanding the pool of insured persons, but it leaves many of the problems inherent in our health care system unresolved. There are important disparities in provision of care that extend beyond the presence or absence of insurance as Angel’s case demonstrates. The ACA doesn’t connect Medicaid across the States, will not guarantee more convenient providers in impoverished areas, does not address transportation or issues such as stigmatization, and does not specifically support many of those interventions mentioned above that can contribute to coordination of care. We should see and applaud the improvements the ACA brings. Yet we all need to realize that more needs to be done to ensure that Americans get the health care they need. Unless we as a society support a system in which real health care access is a reality poor outcomes and preventable morbidity and mortality will continue to plague the health of our nation.
Written by Ashly E Jordan, a DPH Candidate at the City University of New York.