Chances are you have or you know someone who has asthma, hypertension or diabetes. These are serious illnesses that raise morbidity and mortality rates. Medicine alone is not enough to manage these conditions. To start, individuals should eat healthy foods, avoid cigarette smoke, have access to jobs, health care, and safe communities.
But what if you live in a community where there is no grocery store, the air quality is poor, or the unemployment and poverty rates are so high, health is no longer a priority? These conditions are just a few of the realities that impact health for so many individuals. For example, the Morrisania section of the Bronx was once called a “food desert”; a place where grocery stores did not exist and access to fresh fruits and vegetables was inadequate. So exactly how could one eat healthier? In New York, there are some midtown districts where the air quality is at unacceptable levels. What affect does that have on individuals who have asthma and work in those areas? Lastly, there is a direct relationship between poverty and health. Individuals in poor households tend to have worse health outcomes for reasons beyond their control.
How do we improve the health of our society when we know that a prescription for medication does not translate to healthier food on the table, better air quality or employment? What are the lessons learned from our past that can be used to inform our future?
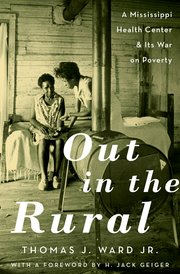
In the book, Out in the Rural: A Mississippi Health Center and Its War on Poverty, Dr. Thomas J. Ward takes us back to the early 1960’s to explore the triumphs and challenges faced by Dr. H. Jack Geiger and others who established the first rural community health center in the United States, the Tufts-Delta Health Center. The Center was established during a time when many African Americans were denied access to health care. When health care was accessible, they had to use the back door, wait in separate rooms or were expected to tell the doctor what their problem was because some doctors refused to touch them. In addition, since emergency care required immediate payment, some died on the hospital steps. Some communities in Mississippi faced astonishing health care challenges that led to the highest infant and maternal mortality rates in the country. But that was all about to change.
Tune in to HealthCetera to hear the conversation with Diana Mason, Kenya Beard, and the author of Out in the Rural: A Mississippi Health Center and Its War on Poverty, Dr. Thomas J. Ward. Find out how the Tufts-Delta Health Center addressed the social determinants of health, provided comprehensive health care, and improved the health of a community. Indeed, the lessons learned 50 years ago could still be used today. So tune in on Thursday, May 11th at 1:00 PM to WBAI, 99.5 FM in NYC or streaming at www.wbai.org.